Understanding COPD and Interstitial Lung Disease
When Darcy was diagnosed with an auto-immunue, auto-inflammatory disease, sarcoidosis, his lungs were in such a bad state he was also diagnosed with COPD and Interstitial Lung Disease.
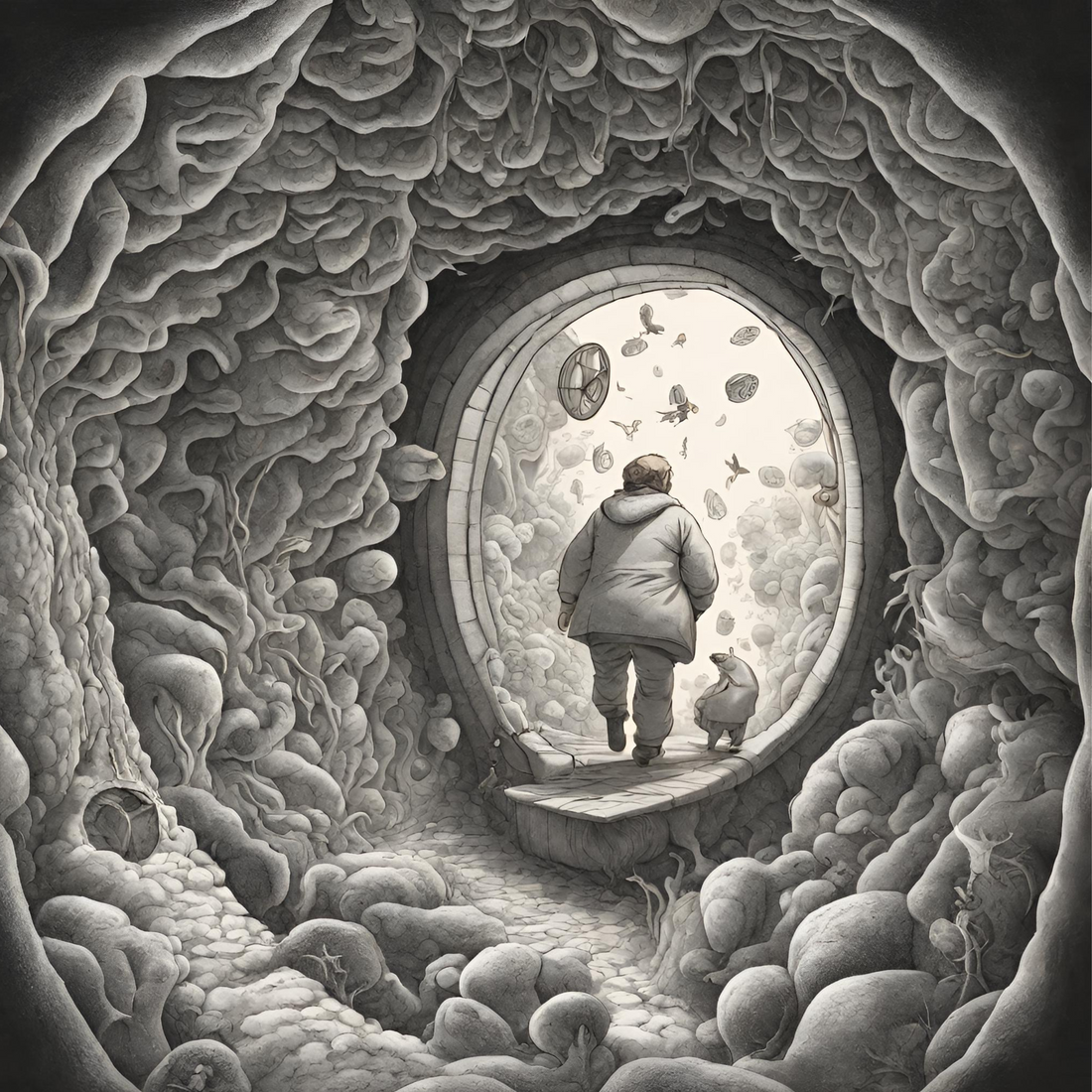
An engineer at the time, his knowledge of the respiratory system was sketchy to say the least, but, being on the spectrum (Darcy has high-functioning autism), he entered an exploratory journey that led him down a very deep biological tunnel to understand what he might do to breathe freely again. Understanding this, also led him to co-found Zestt with me (Anna).
Let’s look at COPD (chronic obstructive pulmonary disease) and Interstitial Lung Disease (ILD) - two common yet distinct pulmonary conditions.
COPD, is an umbrella term which encompasses diseases like chronic bronchitis and emphysema. What characterises COPD is persistent inflammation and mucus production in the bronchial tubes and a narrowing of the air passages, impeding airflow. Emphysema, also entails the gradual destruction of lung tissue, particularly the air sacs responsible for oxygen exchange, leading to decreased lung elasticity and breathlessness. This leads to a multitude of symptoms—shortness of breath, chronic coughing, and wheezing—often exacerbated by smoking or exposure to pollutants.
In contrast, ILD occurs when the delicate fabric of lung tissue becomes scarred and inflamed. Unlike COPD, which primarily affects the airways, Interstitial Lung Disease affects the interstitium—the tissue surrounding the air sacs—leading to stiffness and impaired oxygen exchange. Picture tiny, intricate fibres weaving through delicate lung tissue, becoming scarred and inflexible. This hallmark scarring disrupts the architecture of the lungs, hindering their ability to expand and contract with ease. Shortness of breath (a symptom in both COPD and Interstitial Lung Disease) may occur alongside a dry, persistent cough.
The treatment pathways can diverge for COPD and ILD:
- For COPD, a multifaceted approach is important: bronchodilators and inhaled corticosteroids may help alleviate symptoms, while pulmonary rehabilitation can improve physical endurance and quality of life. Smoking cessation and environmental modifications are critical too.
- For ILD, certain medications like corticosteroids or immunosuppressants may mitigate inflammation and targeted therapies, such as pirfenidone or nintedanib, are also available to slow the progression of fibrosis in specific ILD subtypes. Oxygen therapy and pulmonary rehabilitation also support better lung health.
For both diseases, lifestyle changes can make an impact – see previous blogs we have written on this (read more here and here).
Since his diagnosis, Darcy has improved his lung capacity significantly from 62% to 86% (Darcy is happy to share his medical data with anyone interested in learning more). He has done this through a combination of pharmaceuticals and lifestyle changes (including Zestt supplements) and has managed to reduce the number of pharmaceuticals he takes on a daily basis from 26 to 4.
Does he still have bad days?
Yes, lung scarring cannot be repaired, and he is still immunocompromised, the sarcoidosis also affected other organs in his body. But if you asked him about the exploratory and physical journey that led him to be where he is now – he states “I’m just trying not to die.”
Darcy trying not to die has given him (and Zestt) the purpose of supporting others who find themselves with chronic inflammation and disease.
It’s never too late to make small changes.
All the best, Anna and Darcy.
If you would like to discuss any of this further, please contact Darcy or Anna (who you can contact at +64 27 599 2255 or +64 27 4861418 respectively) or via info@zesttwellness.com.